Before, Between & Beyond Pregnancy
Women’s Health Matters.
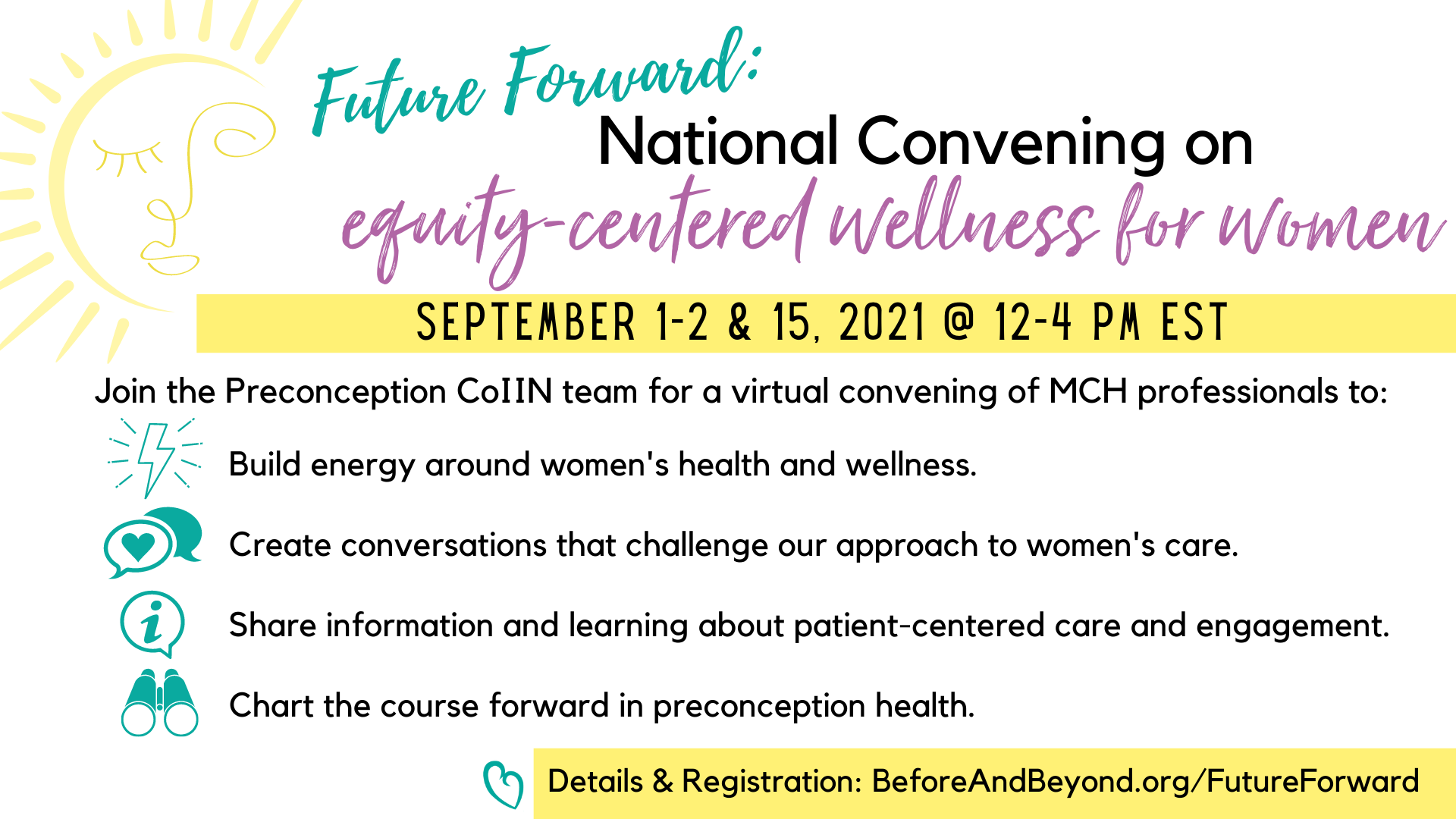
The Show Your Love Today Initiative’s Future Forward: National Convening of Equity-Centered Women’s Wellness sessions took place on September 1st, 2nd, and 15th, 2021. The purpose of this national virtual summit was to build energy, create conversation, share information and learning, and chart the course forward in ‘preconception health.’
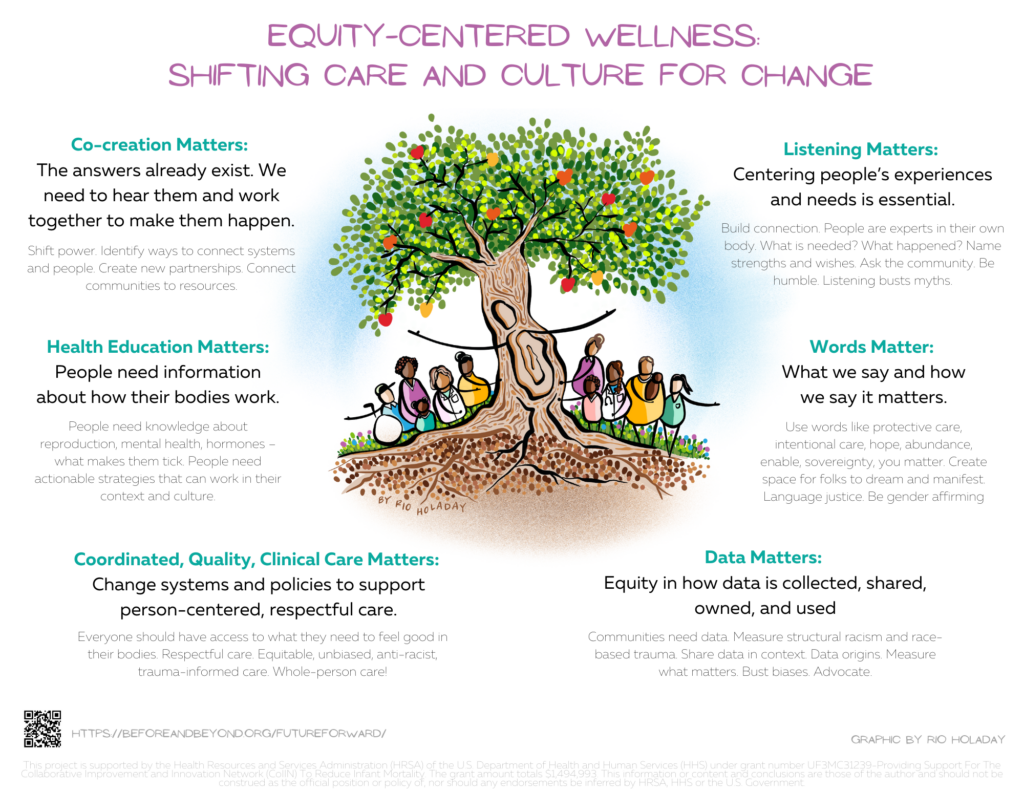
Below graphic is a summary of our Future Forward discussions.
Questions? Email SuzanneW@med.unc.edu.
Session Recordings – Rewatch!
Session Recordings – Rewatch!
Session Graphic Notes
Session Graphic Notes
Rio Holaday has created live, inspired art for each of our sessions. Click to engarge the graphic note images.
Day 1 – September 1st
Session 1 – Setting the Stage
 Session 2: Opportunity for Change
Session 2: Opportunity for Change 
Day 2 – September 2nd
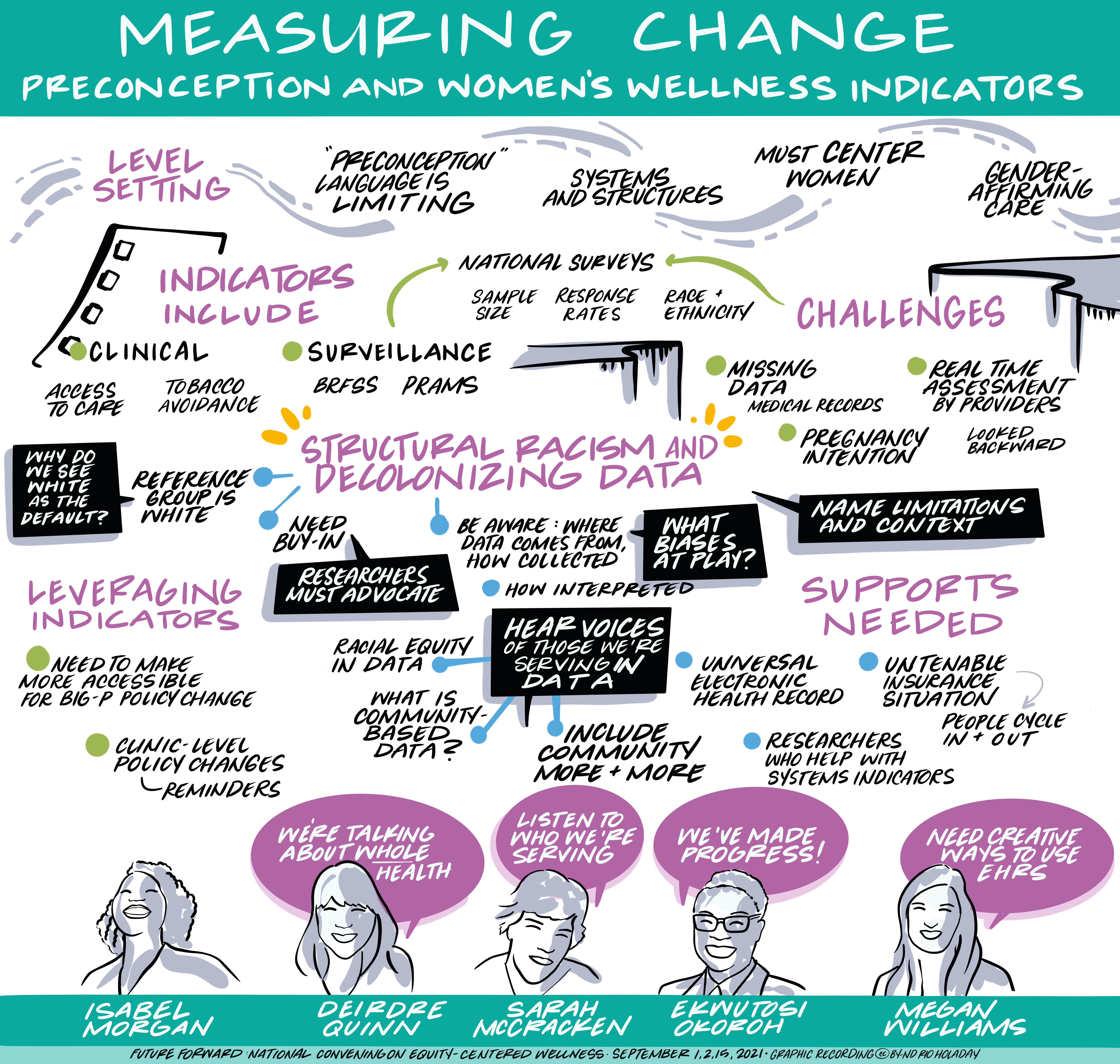 Session 3: Measuring Change – Preconception and Women’s Wellness Indicators
Session 3: Measuring Change – Preconception and Women’s Wellness Indicators
Session 4: Reproductive Life Planning: Best Practices and Implications for Patient Care and Program Planning
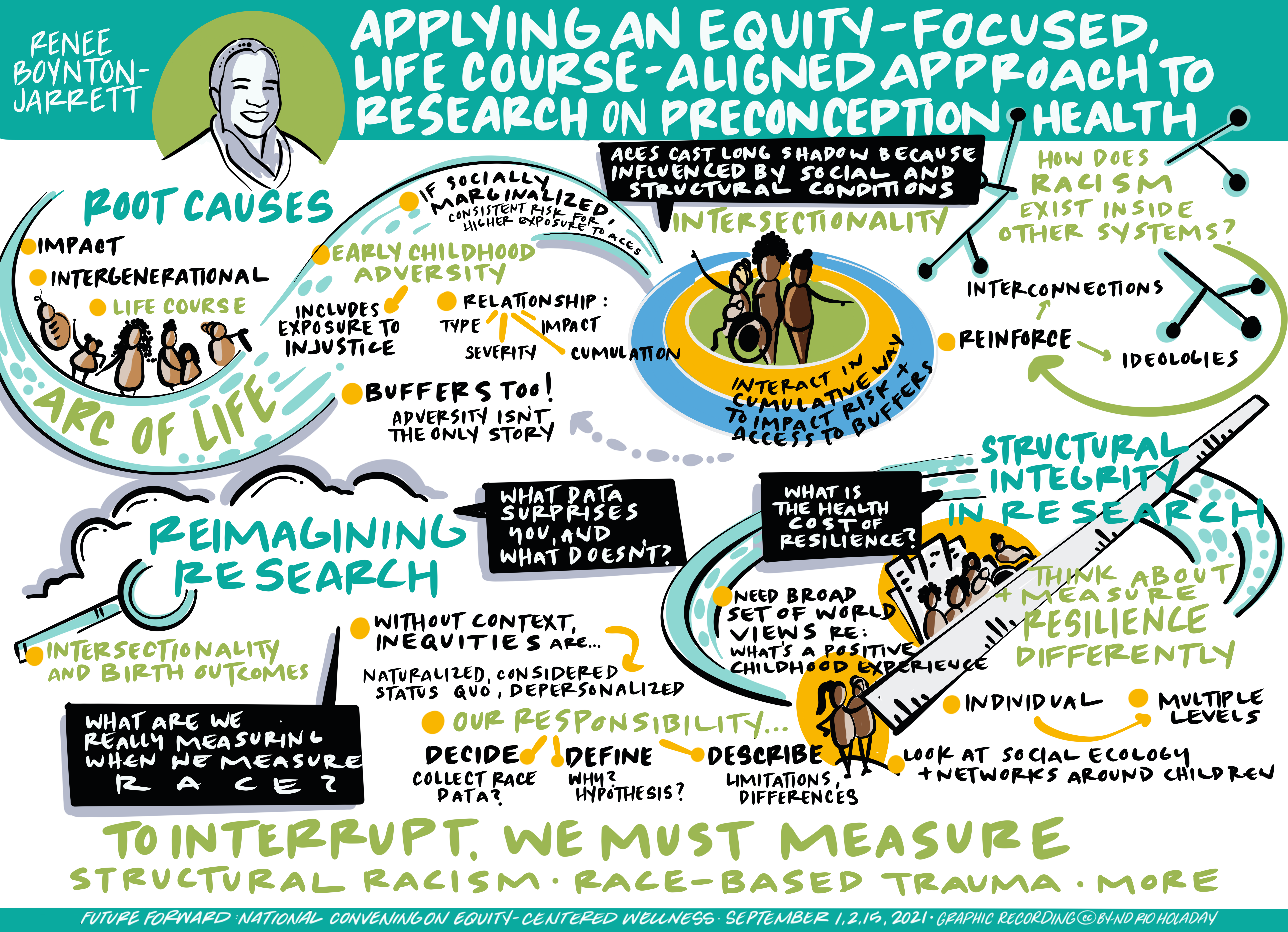 Session 5: Applying an Equity-Focused, Life Course-Aligned Approach to Research on Preconception Health
Session 5: Applying an Equity-Focused, Life Course-Aligned Approach to Research on Preconception Health
Day 3 – September 15th
 Session 6: Revisiting Preventive Visits for Women as a Title V National Performance Measure and Unique Opportunity
Session 6: Revisiting Preventive Visits for Women as a Title V National Performance Measure and Unique Opportunity
Session 7: Transforming Patient Care and Engagement Using Social Media
Session 8: Vision Forward: New Ideas for Advancing an Equity-Aligned Approach to Wellness and Wellbeing
Program
Program
September 1st
Sarah Verbiest, Erin McClain, Katherine Bryant, Suzanne Woodward, Rio Holaday, Chemyeeka Tumblin, Eilish Neely, Vanessa Lee
Join us at 1:15pm ET for a welcome and stage setting as we begin the Future Forward Conference.
Omar Young, Narges Farahi, Sarah Verbiest, Chemyeeka Tumblin, Eilish Neely, Jussica Haynes, Kennedy Bridges – moderated by Rio Holaday
This session will feature a lively conversation across a diverse group of leaders about how we define these terms, what they mean to us, why they matter, and what a future-forward vision could look like. Rio Holaday, graphic facilitator, will moderate this session using her art skills to help us move the conversation to the next level.
Kay Johnson, Diana Ramos, Christie Allen, Lekisha Daniel-Robinson, Naomi Clemmons
Facilitated by Kay Johnson, lead author of the original 2006 publication on CDC Recommendations on Preconception Health, this session will identify areas where we have made significant strides forward in improving women’s health and areas where more work needs to be done. This session features a panel of experts who will have a candid conversation about levers for change and what needs to happen to push them forward.
Resources to review:
The Medicaid Coverage Gap and Maternal and Reproductive Health Equity
The Commonwealth Fund interactive maps on state policies and maternal health
All are welcome to join this discussion – cameras on or off.
During this session, all attendees will have an opportunity to speak with presenters and discuss today’s sessions. We will review ideas shared on Jamboard. Be sure to add your ideas and insights to our Future Forward Jamboard throughout the conference.
September 2nd
Isabel Morgan, Sarah McCracken, Megan Williams, Deirdre Quinn, Ekwutosi Okoroh
At the end of this session, participants will be able to describe current indicators and strategies for measurement of preconception health at the clinical, state, and federal levels. Additionally, panelists and attendees will have an opportunity to share feedback about the next steps to move forward in this space.
Resources to explore:
- Urban Inst Do No Harm Guide
- Health_Equity_Style_Guide_CDC reducing stigma
- Health Care System Measures to Advance Preconception Wellness – Frayne et al – https://journals.lww.com/greenjournal/Fulltext/2016/05000/Health_Care_System_Measures_to_Advance.8.aspx
- Preconception Health Indicators for Public Health Surveillance – Robbins et al – https://www.liebertpub.com/doi/10.1089/jwh.2017.6531
- Making the Case: The Importance of Using 10 Key Preconception Indicators in Understanding the Health of Women of Reproductive Age – Kroelinger et al – https://pubmed.ncbi.nlm.nih.gov/29630430/
- Disparities in Preconception Health Indicators — Behavioral Risk Factor Surveillance System, 2013–2015, and Pregnancy Risk Assessment Monitoring System, 2013–2014 – Robbins et al – https://www.cdc.gov/mmwr/volumes/67/ss/ss6701a1.htm
- Core State Preconception Health Indicators — Pregnancy Risk Assessment Monitoring System and Behavioral Risk Factor Surveillance System, 2009 – CDC – http://beforeandbeyond.org/wp-content/uploads/2018/05/ss6303.pdf
- Surveillance Indicators for Women’s Preconception Care – Journal of Women’s HealthVol. 29, No. 7 Alys Adamski, Peter S. Bernstein, Sheree L. Boulet, Farah M. Chowdhury, Denise V. D’Angelo, Dean V. Coonrod, Daniel J. Frayne, Charlan Kroelinger, Isabel A. Morgan, Ekwutosi M. Okoroh, Christine K. Olson, Cheryl L. Robbins, Sarah Verbiest. Published Online:9 Jul 2020 https://doi.org/10.1089/jwh.2019.8146
- Callegari LS, Edmonds SW, Borrero S, Ryan GL, Cusack CM, Zephyrin LC. Preconception Care in the Veterans Health Administration. Semin Reprod Med. 2018 Nov;36(6):327-339. doi: 10.1055/s-0039-1678753. Epub 2019 Apr 19. PMID: 31003248.
Erin McClain, April Lyons-Alls, Daniel Frayne, Debra Stulberg, Meredith Manze, Patty Cason
During this session, panelists will describe varied approaches to asking patients about their pregnancy intentions, explore common challenges and opportunities when providing responsive care, discuss potential pitfalls – both clinically and programmatically – and share their views of what’s on the horizon. Attendees will have the opportunity to ask questions of the panelists and weigh in on future directions in the field.
Resources to review for this session:
- Delaware Preconception CoIIN Updates – View Slides
- PATH Resources Client-Centered Reproductive Goals & Counseling Flow Chart: https://rhntc.org/sites/default/files/resources/rhntc_path_clnt_cntrd_cnslng_2021-03.pdf
- Efficient Questions for Client-Centered Contraceptive Counseling: https://rhntc.org/sites/default/files/resources/fpntc_eff_qs_path_card_2019-03.pdf
- PATH Counseling Skills Demonstration: https://www.envisionsrh.com/counseling-movies
- Tips for Providing Patient-Centered Contraceptive Care Using Telehealth: https://www.nationalfamilyplanning.org/telehealth-video-guide
- CDC A Guide to Taking a Sexual History: https://www.cdc.gov/std/treatment/sexualhistory.pdf
- ICAN! Illinois Contraceptive Access Now: https://ican4all.org/
- Power to Decide – One Key Question Online: https://powertodecide.org/one-key-question
- University of Chicago, Reproductive Health Outcomes and Disparities (RHOADS) Research: https://familymedicine.uchicago.edu/research/reproductive-health-outcomes-and-disparities-rhoads-research
- Meredith Manze’s Research Publications: https://scholar.google.com/citations?user=9y9PMEkAAAAJ&hl=en
- Delaware Resources: General Information: Delaware Thrives | Helping Delaware Stay Healthy. Let’s All Thrive (dethrives.com)
- Healthy Women Healthy Babies Program Women | Healthy Babies – Delaware Thrives (dethrives.com)
- HWHB SDOH Grantees: Healthy Women Healthy Babies Zones Mini-Grants | Thriving Communities – Delaware Thrives (dethrives.com)
- RLP Women: Overview | My Life My Plan: Women. – Delaware Thrives (dethrives.com)
- RLP Teens: Delaware Thrives | My Life My Plan: Teen (dethrives.com)
- Man Up Plan Up: Do The Math | Man Up Plan Up – Delaware Thrives (dethrives.com)Preconception Peer Education Program: Peer Educators | Thriving Communities – Delaware Thrives (dethrives.com)DHMIC Strategic Initiatives: Strategic Initiatives | Delaware Healthy Mother and Infant Consortium – Delaware Thrives (dethrives.com)Preconception CoIIN: Preconception COIIN | Strategic Initiatives – Delaware Thrives (dethrives.com)
Renée Boynton-Jarrett
Hear from Dr. Renée Boynton-Jarrett as she centers our discussion around an equity-focused approach to our research, collaborations, and programs.
All welcome to join the discussion – cameras on or off. Be sure to add your ideas and insights to our Future Forward Jamboard throughout the conference.
During this session, we will have an opportunity to speak with presenters and discuss today’s sessions. We will review ideas shared on Jamboard.
September 15th
Keriann Uesugi, Andria Cornell, Giannina Ong, Kristina Wint
The Title V Maternal and Child Health Services Block Grant program is a federal / state partnership with the goal to support the health and well-being of all mothers, children, and families. In 2019, the Block Grant provided access to health care and public health services for an estimated 60 million people. Several years ago, a new Title V national performance measure was introduced: National Performance Measure #1: Percent of women, ages 18 through 44, with a preventive medical visit in the past year (data source, Behavioral Risk Factor Surveillance System). During this session, speakers will share the history and original intent of NPM1, the federal and state/territory experience implementing the NPM over the years, and considerations for the future. After this foundational presentation and initial discussion, speakers will then engage the audience in an interactive exploration of opportunities to innovate with the NPM to advance equity-centered wellness. Topics that may be covered through group participation could include re-imagining access to care to be more than geographic access; an exploration of who provides holistic care for girls, women, persons born female, and persons who identify as female; and opportunities to leverage state performance measures and cross-cutting measures.
Charis Chambers, MD, Pediatric & Adolescent Gynecologist, The Period Doctor, LLC
Dr. Charis Chambers, well-known as “The Period Doc,” will present ‘Social Media Basics for the Health Professionals.’
Dr. Chambers will share how to use social media to achieve transformative patient engagement. She will review the evolution of social media and the differences in the available platforms, discuss the literature supporting the intersection of healthcare and social media, share her personal social media process and growth, and propose potential ways for clinicians to start making their own mark on social media.
Learn more about Dr. Chambers at www.ThePeriodDoc.com.
Kanika Harris, Natalie Hernandez, Narges Farahi, Fofie Akoto
This closing session will be a conversation to generate new ideas for taking this important work forward. Panelists will challenge words such as “at risk” and highlight the barriers people face when they lack access to information, choices, and resources. Then they will talk about their fresh ideas – like considering relational wealth, elevating person-centered care and group approaches, and sharing about some of the new work they are leading. Audience members will be able to chat in and share their innovative ideas too. This will be a powerful final session that will leave participants with energy and true future forward thinking!
Sarah Verbiest, Katherine Bryant, Erin McClain, Ana Cabello-De la Garza, Suzanne Woodward
Speakers
Speakers

Dr. Charis Chambers also known as The Period Doctor is an OB/GYN with fellowship training in Pediatric & Adolescent Gynecology. She is a speaker, lover of God, medicine, and most of all, a person who is changing the cycle.
She launched her social media platform, The Period Doctor, in the summer of 2019, after recognizing an unmet need for medically accurate women’s health information and minority physician representation in social media outlets.
Get to know, follow, and learn more about Dr. Chambers here.

Rio Holaday (she/her) is a graphic recorder and facilitator based in San Francisco on Ohlone land.
Rio Holaday is a graphic recorder and facilitator. She has a background in social justice and public health, and is a Culture of Health Leader with the Robert Wood Johnson Foundation. Rio became a graphic recorder after a career in public health because she believes in the importance of witnessing, making people feel heard, and making conversations accessible in order to make change.
Rio was formerly the Director of HOPE Collaborative, which organizes black and brown communities in Oakland around equitable health policies, and a Senior Policy Analyst at ChangeLab Solutions, which uses policy and planning tools to create healthier communities. She co-founded Rebel Ventures, a social enterprise that works with high school students to make healthy snacks to sell in corner stores and schools, and conducted research on food access in Philadelphia. Rio is a former Fulbright Scholar and worked in refugee resettlement in Vermont. She received her MPH from the University of Pennsylvania, MA in Forced Migration from the University of the Witwatersrand (VIT-vahters-rand), and BA from Wesleyan University.

Narges Farahi is a family medicine physician and longtime champion for person-centered and family-centered care. After completing family medicine residency training at UCSF and obstetrics fellowship at Santa Clara Valley Medical Center, Dr. Farahi joined the faculty at UNC, where she now serves as an Associate Professor and the Director of the Family Medicine Maternal and Child Health Service. Dr. Farahi’s heart is in community health, and her outpatient practice is at Prospect Hill Community Health Center, a rural federally qualified health center. Prior to her current role, Dr. Farahi served as the medical director of the NC Farmworker Health Program.
Dr. Farahi’s clinical interests include providing seamless care for people with the capacity for pregnancy across the continuum of care, including before, between and after pregnancies. She is committed to providing trauma-informed care, supporting people and families to meet their reproductive goals, and using community engagement and quality improvement strategies to help health care practices and systems better meet the needs of patients and families. She has been a leader in implementing enhanced access to comprehensive contraception options and the IMPLICIT interconception care model in the primary care setting in her region and believes deeply in the unique role that family physicians have in improving the health of the families they care for through longitudinal and cross-generational care. Her goal is to help center the voices of patients and families from marginalized communities and build partnerships with patients and communities to improve health.

Dr. Omar M Young completed his undergraduate studies at Washington University in St. Louis in Biology and French in 2004. He went on to receive his medical degree from Columbia University in the City of New York. He was a fellow in Maternal-Fetal Medicine at Magee-Womens Hospital/UPMC. Dr. Young’s academic interests include medical education/simulation, inter-professional practice, cardiovascular diseases in pregnancy, and health care disparities. He is currently an associate professor in the Department of Obstetrics and Gynecology in the Division of Maternal-Fetal Medicine and Ultrasound at UNC Chapel Hill, where he serves as the Associate Residency Program Director.

Lekisha Daniel-Robinson, MPH, is an IMI health policy associate and project director for the reducing disparities through payment and health system reform project. Prior to joining IMI, she served as a technical director in the Division of Quality and Health Outcomes within the Center for Medicaid and CHIP Services (CMCS) at the Centers for Medicare and Medicaid Services (CMS).

Naomi Clemmons has over 22 years of experience in maternal and child health. Naomi’s work focuses on the drivers of health disparities that perpetuate poor health outcomes experienced by women, children, and families. On a federal level, Naomi is senior technical advisor or senior evaluation analyst on various projects including Supporting Healthy Start Performance Project, and oversaw technical assistance to 100 Healthy Start grantees to ensure program effectiveness in achieving the goals to reduce infant mortality and health disparities, and improve perinatal health outcomes; CDC Teen Pregnancy Prevention initiative on social determinants of teen pregnancy; and the Maternal and Child Health Bureau Division of Services for Children with Special Health Needs, Building Capacity for Performance Measurement and Quality Improvement for State Partners Serving Children and Youth with Special Health Needs supporting grantees’ efforts to further systems integration to improve the health outcomes of children and youth with special health care needs. Naomi works closely with State Title V programs conducting comprehensive strengths and needs assessments and supporting action planning processes and special initiatives.
Dr. Diana E. Ramos, is the Assistant Deputy Director for Chronic Disease prevention in the Center for Healthy Communities for the California Department of Public Health. She is an adjunct Assistant Professor, at the Keck University of Southern California School of Medicine Dr. Ramos serves as the chair for the American College of Obstetricians and Gynecologist, California & Ecuador (IX) District, Serves as the Co-Chair for the Women’s Preventive Service Initiative implementation committee, and is secretary for the executive board of the National Hispanic Medical Association.
She serves on many national and international health improvement and quality committees. Her areas of expertise include health equity /disparities, social determinants of health, wellness, and quality improvement in healthcare delivery. Dr. Ramos has written and contributed numerous articles to the obstetrics and gynecology and public health literature and has lectured in Spanish and English, locally, nationally, and internationally. She has received numerous innovation awards for her work in health, technology, and communication.
Recent awards include 2020 UCI Latino Excellence and Achievement Award, 2019 UC Irvine Dynamic Womxn Award for Academic Achievement, 2018 National Hispanic Medical Association Fellow of the Year, Let’s Get Healthy California’s 2017 Innovation Challenge Finalist, 2017 Global Health& Innovation: Semifinalist for Choose Health LA MOMs 2016 Health Officers Association of California Public Health Communications Award and 2016 American Congress of Obstetricians and Gynecologists District Service Award.
Dr. Ramos received her medical degree from the University of Southern California with honors and completed her residency training in obstetrics and gynecology at Los Angeles County-University of Southern California Medical Center. She received her MBA from the UCI Paul Merage School of business with an emphasis in entrepreneurship and innovation and her master’s in public health from the University of California, Los Angeles. Dr. Ramos completed her undergraduate degree, a BA in Communications, Arts & Science from the University of Southern California

Christie Allen MSN, RNC-NIC, CPHQ, C-ONQS is the Senior Director, Quality Improvement and Programs. She provides clinical support to and supervision of the AIM Program and other affiliated grants at ACOG. Prior to this role, Christie served as the Associate Director of Clinical Quality for ACOG, as a quality coordinator for a Planned Parenthood affiliate, and as the coordinator of a statewide Medicaid program for people with substance use disorder in pregnancy. Christie has practiced as a clinical bedside nurse for over 20 years in adult, pediatric, and neonatal intensive care and inpatient obstetrics, as well as a lactation consultant and holds and advanced degree in health policy.

Isabel Morgan, MSPH, is a PhD student in Maternal and Child Health and Epidemiology at the UNC Gillings School of Global Public Health, where she studies the effects of structural racism on Black maternal health outcomes. Prior to her doctoral studies, Isabel was as a Reproductive Epidemiology Fellow at the CDC, where she evaluated evidence for the U.S. Medical Eligibility Criteria for Contraceptive Use. Isabel is a free spirit who enjoys traveling to the Caribbean and Africa, dancing to Soca and House music, and being a loving auntie to her precious niece and nephew.
Isabel received a BA in Anthropology from Mount Holyoke College and MSPH in Population, Family and Reproductive Health from the Johns Hopkins Bloomberg School of Public Health.

Johnson Group founder and president, Kay Johnson, has been a leader in health policy for women, children, and families for 35 years. She has been active in Medicaid and children’s health policy at the federal and state levels since 1984 and has served as an advisor to more than 40 state health and/or Medicaid agencies. Her expertise encompasses a wide range of maternal and child health issues. Formerly, she served as the national policy director at March of Dimes, and director of health policy at the Children’s Defense Fund. Prior to her policy career, Ms. Johnson worked with low-income families in early care and education settings.

Deirdre A. Quinn, PhD, MSc, MLitt, is an Advanced Research Fellow in Women’s Health with the Center for Health Equity Research and Promotion (CHERP) at the VA Pittsburgh Healthcare System and Adjunct Instructor of Medicine in the Division of Internal Medicine at the University of Pittsburgh. Dr. Quinn earned her doctorate in Family Science from the University of Maryland School of Public Health. She also holds an MSc in Gender and Social Policy from the London School of Economics & Political Science and an MLitt in Creative Writing from the University of St. Andrews.
Dr. Quinn’s research explores individual- and community-level influences on sexual and reproductive health. Her VA HSR&D-funded Career Development Award proposes to examine how links between women Veterans’ pre-pregnancy health risks and healthcare experiences, social characteristics, and maternal outcomes can inform interventions to improve women Veterans’ healthcare.

Dr. Ekwutosi Okoroh, is a Lieutenant Commander (LCDR) in the United States Public Health Service and is currently the Team Lead for the Maternal and Child Health Epidemiology Program (MCHEP), overseeing the scientific work of Senior Maternal and Child Health (MCH) Epidemiologists assigned to 13 state health departments. Dr. Okoroh was also the first ever Centers for Disease Control and Prevention (CDC) Senior MCH Epidemiologist assigned to a Medicaid program in the state of Louisiana (LA) where she lead a 40 member team on a statewide study on the public health and financial burden of neonatal abstinence syndrome and substance use disorder among LA Medicaid-enrolled infants, prompting legislation on NAS prevention and treatment recommendations. She also supervised and directed LA’s 5 managed care organizations on several performance improvement projects. Dr. Okoroh joined CDC in 2010 as an Epidemic Intelligence Service Officer in the Division of Blood Disorders in the National Center on Birth Defects and Developmental Disabilities where her work focused on addressing bleeding and thrombotic issues among women of reproductive age. She currently holds 2 adjunct facility positions as a practicing Obstetrician/Gynecologist (OB/GYN), and provides vital clinical care to women.
She received her MD and MPH from Tufts University School of Medicine and completed her residency in OB/GYN at Phoenix Integrated Residency in Obstetrics and Gynecology at the Clarkston Community Health Center and the Harriet Tubman Women’s Clinic.

Latrice Rollins is an Assistant Professor at Morehouse School of Medicine (MSM) in the Department of Community Health and Preventive Medicine, where she embraces a community-based participatory approach for all projects she leads. Dr. Rollins is also a Robert Wood Johnson Culture of Health Leader, seeking to build a culture of health and advance health equity for African American fathers. Dr. Rollins was an award-winning program analyst for the U.S. Department of Health & Human Services Office of Inspector General, evaluating national programs that impact the most underserved populations. Dr. Rollins also worked for Georgia’s Office of Child Support Services and the Georgia Fatherhood Program. She presents at state and national conferences on father engagement and provides father engagement training for practitioners in various sectors. She is the editor and one of many authors of the book, Engaging and Working with African American Fathers: Strategies and Lessons. Dr. Rollins received a bachelor’s in sociology from Spelman College and a master’s and doctorate in social work from the University of Georgia.

Kanika Harris, PhD, MPH,Black Women’s Health Imperative, Director of Maternal Health – Dr. Harris currently serves as the director of maternal health for the Black Women’s Health Imperative. She is a behavioral health scientist, with a special focus on health equity, maternal health and women’s health. She is a mother of 3, near miss survivor, doula, and birth justice advocate. She also serves as the Maternal Health Equity Advisor for the State of Maryland and the public health expert for the lactation commission in Washington DC.
Dr. Harris is co-directing and producing a documentary called “Listen to Me” which explores four women at the frontlines of the Black maternal health movement walking the tightrope of racism and birth in America funded by Black Public Media.
She received her master’s degree in public health and international development from Morehouse School of Medicine and her PhD in Health Behavior and Health Education from the University of Michigan.

Kristina Wint, MPH is the Program Manager for Women’s Health at AMCHP. A graduate of the University of Pittsburgh Graduate School of Public Health, Ms. Wint has special interest in understanding the relationship between health inequities and disparities and learning how the field of public health can restructure systems to stop inequities from persisting. At AMCHP, she manages the women’s health portfolio, including representing AMCHP on the Executive Team of ACOG’s Alliance for Innovation on Maternal Health (AIM), supporting AMCHP’s efforts to build capacity of maternal mortality review committees through partnership with the CDC’s ERASE MM Initiative, leads an integration test of the AIM Reducing Peripartum Racial/Ethnic Disparities Bundle co-created with community partners, and supports the Merck for Mother’s funded Safer Childbirth Cities Initiative Community of Practice.

Giannina Ong, MA is a Maternal Health Program Associate at AMCHP supporting Merck for Mother’s Safer Childbirth Cities Initiative and the accompanying Community of Practice. She is a master’s graduate of the University of Toronto where she focused on women and gender studies. Her culminating master’s thesis explored the experience of immigrant women during the postpartum period, and she has worked on numerous qualitative projects, designing, implementing, and analyzing data to better understand and empathize with challenging and complex problems.

Natalie D. Hernandez, PhD, MPH, Assistant Professor, Department of Community Health and Preventive Medicine; Executive Director, Center for Maternal Health Equity -Dr. Hernandez is an Assistant Professor in the Department of Community Health and Preventive Medicine and the Executive Director of the Center for Maternal Health Equity at Morehouse School of Medicine. Dr. Hernandez has a broad background in community-based participatory research (CBPR), women’s health inequities, health policy, and social determinants of health. She has more than 15 years of experience in developing community partnerships and implementing CBPR that engages with diverse stakeholder groups. Dr. Hernandez has served as the Principal Investigator (PI) or co-investigator on numerous university, private, foundational, and NIH-funded grants focused on women’s health inequities. In 2019, she helped to establish the Morehouse School of Medicine’s Center for Maternal Health Equity and serve as the PI to conduct interdisciplinary translational research aimed at advancing the understanding, prevention, and reduction of maternal mortality or morbidity among ethnoracial minority women and underserved populations. She is Co-PI on numerous projects examining the integration of technology in addressing maternal health inequities and improving reproductive and sexual health outcomes for ethnoracial minority women. Dr. Hernandez currently sits on Georgia’s Maternal Mortality Review Committee, Georgia PRAMS Steering Committee, and on various maternal and child health organizations including Postpartum Support International-Georgia Chapter Advocacy Group and Georgia Maternal Health Stakeholder Group. She also sits on national organizations including the American Public Health Association Committee on Health Equity, Health Disparities Taskforce of the National Preeclampsia Foundation, and many others. Dr. Hernandez has presented her work at various international, national, state, and local conferences. Dr. Hernandez received her Master of Public Health from Emory University’s Rollins School of Public Health and a Bachelor of Arts in anthropology from Stony Brook University in New York. She earned her PhD in public health as well as a graduate certificate in interdisciplinary women’s health from the University of South Florida

Fofie Akoto, MD – As the daughter of two amazing artists who were also elite educators and incredible people, I am a very well-rounded human being, with a passion for living life to the fullest. I have always wanted to be a physician, but my family made certain that I pursued all of my interests from the time that I was young. I love art, culture and science, and I am in constant awe of what the human body is capable of. I chose the practice of medicine as a profession because it is the perfect combination of art and science, and healing is something that I am passionate about. I was born and raised in one of the best cities on earth, Washington, D.C. I have also lived in Philadelphia, Penn. and Nashville, Tenn., and ultimately settled here in Atlanta in 2013. I am a mother, an artist, a scientist and I thoroughly enjoy my job as a physician.

Dr. Uesugi is the Health Scientist in the DSCH, in the MCHB. Dr. Uesugi is a maternal and child health epidemiologist who leads the reporting of the Title V Maternal and Child Health Block Grant National Outcome and Performance Measures and supports technical assistance to the States around the Performance Measurement Framework and use of evidence-based/informed practices. Prior to joining MCHB, Dr. Uesugi was a Research Assistant Professor at the University of Illinois at Chicago School of Public Health where she led applied MCH epidemiology research and evaluation projects for state and federal programs. Her earlier work focused on global and domestic Maternal and Child Nutrition research in academic and industry settings. She holds a Ph.D. in Human Nutrition from Cornell University and an M.P.H. in Epidemiology and Biostatistics from the University of Illinois at Chicago School of Public Health.

Andria Cornell, MSPH is the Associate Director for Women’s and Infant Health at the Association of Maternal & Child Health Programs, or AMCHP. AMCHP is a national resource, partner and advocate for state public health leaders and others working to improve the health of women, children, youth and families. Ms. Cornell oversees a dynamic team and an extensive portfolio of grant-funded efforts centered in racial equity and bridging public health and clinical care in women’s health, improving birth outcomes, care and support for the mother-baby dyad, and transition to early childhood systems. Ms. Cornell has worked across the academic, federal and nonprofit sectors advancing maternal and child health in the fields of public health, research, and health care. She has a Master of Science in Public Health in reproductive, perinatal and women’s health and a certificate in public health informatics from Johns Hopkins Bloomberg School of Public Health.


Patty Cason is a family nurse practitioner, trainer, and educator with a specialty in sexual and reproductive health. She has practiced for 38years in a wide variety of clinical and academic settings and is a contracted consultant to training agencies, non-profits, and state departments of health across the United States. Patty developed the “PATH” framework for person-centered reproductive goals and contraception counseling. She is an editor of the 21stEdition of contraceptive Technology for which she wrote a seminal chapter on reproductive goals and contraception counseling. Patty serves on the ASCCP Board of directors,theNational Medical Committee for Planned Parenthood Federation of America, and several advisory boards including the Clinical Training Center for Family Planning. Patty loves making videos to demonstrate counseling skills. Other publications include research and opinion pieces in peer-reviewed journals, nationally utilized online learning courses, textbook chapters, clinical protocols, job aids, and manuals.

April Lyons-Alls, RN, MSN, MPA – April L. Lyons-Alls currently serves as the Women, Infants and Families Nurse Consultant to the Delaware Healthy Mother and Infant Consortium and Division of Public Health supporting the Preconception CoIIN, Black Maternal Health, Preconception Peer Educator and Well Woman Initiatives. Ms. Lyons-Alls has been in nursing practice for more than 25 years working in a variety of public and private sectors as well as academe. Ms. Lyons-Alls holds a Master of Science degree in Nursing from Thomas Jefferson University with a specialty area in Community Systems Administration as well as a Master’s in Public Administration from Delaware State University.
Ms. Lyons-Alls also holds the distinction of being selected to the inaugural class of the Centers for Disease Control and Prevention’s National Leadership Academy for the Public’s Health. She is a member of multiple honor societies which include Sigma Theta Tau International Honor Society of Nursing, Pi Alpha Alpha Honor Society for Public Affairs and Administration, Sigma Pi Alpha, and Golden Key International Honor Society

Debra Stulberg, MD, MAPP, is Associate Professor and Chair of Family Medicine at the University of Chicago. She joined the University of Chicago faculty in 2007, with a primary appointment in Family Medicine and secondary appointments in Obstetrics & Gynecology Section of Family Planning & Contraceptive Research, and the MacLean Center for Clinical Medical Ethics. Dr. Stulberg graduated from Harvard Medical School and completed her Family Medicine residency at West Suburban Hospital in Oak Park, Illinois. She received a Master of Arts in Public Policy from the University of Chicago, where she also completed fellowship training in Primary Care Research and Clinical Medical Ethics.
Her research focuses on reproductive health service delivery in the United States. This includes studies on incorporating reproductive health in primary care, addressing racial and socioeconomic disparities in pregnancy outcomes, and understanding how religious healthcare institutions affect care delivery. She directs the Reproductive Health Outcomes and Disparities (RHOADs) Research Group and co-directs the Research Consortium on Religious Healthcare Institutions. Dr. Stulberg provides patient care at a federally qualified health center on Chicago’s south side.

Since July 2018, Dr. Frayne has served as President of MAHEC. He joined the MAHEC Department of Family Medicine in 2006 and held several leadership positions including Medical Director, Assistant Residency Director, and Medical Director of the Department of Continuing Professional Development and the Simulation Center. 
He attended Boston University and the University of California at Irvine College of Medicine, and completed a Family Medicine Residency at Lancaster General Hospital in Pennsylvania. He then spent four years as a rural primary care physician in Linville, North Carolina. He is an Associate Professor of Family Medicine with UNC-Chapel Hill School of Medicine and is a clinical preceptor for medical students at the UNC School of Medicine Asheville Campus.
Preconception healthcare and advocating for women’s health and improved birth outcomes is an area of great interest to Dr. Frayne. He has been involved in grant-funded collaborations to expand the IMPLICIT Interconception Care model and state and federal Preconception COIIN projects. He has served as a member of the NC State Preconception Health Strategic Planning Team since 2016, is the co-chair of the clinical working group of the National Preconception Health and Healthcare Initiative, and sits on multiple national steering committees focused on improving reproductive health for women. He has collaborated with colleagues to publish numerous articles on this topic and is a presenter at state and national conferences.
Dr. Frayne’s vision is to improve the health of the community by impacting the system from the ground up, both personally and professionally. He believes that the health of our community will be transformed if we focus on healthcare through an intergenerational lens – improving the health of women before pregnancies to achieve a healthier mother and child, and ultimately a healthier family and community. We can only do this well if we transform the way we deliver healthcare. Transformation can happen by focusing on quality outcomes and population health, expanding beyond the clinic structure and into the community AND dedicating ourselves to ending racism and creating equity for all.

Sarah McCracken, MPH, State Systems Development Initiative (SSDI) Project Coordinator – Sarah McCracken works as the State Systems Development Initiative Project Coordinator for the Women’s and Children’s Health Section in the NC Division of Public Health. In this role, she coordinates the annual submission of the MCH Block Grant, assists with the Title V Needs Assessment, and provides data support to various committees and work groups. Sarah received her Master of Public Health degree from Boston University and served in the US Peace Corps in Togo, West Africa.

Megan Williams is a Research Associate at the Collaborative for Maternal and Infant Health at UNC-Chapel Hill, where she works on a variety of maternal and child health issues. Her work includes the provision of training and technical assistance in maternal and child health issues to providers around the state of North Carolina. She recently led a team in a UNC-MAHEC partnership award project analyzing preconception health indicators in the EHR at both sites. Her previous work has been with Duke University, and several statewide and local nonprofit organizations and health departments. A common thread throughout her experience is a dedication to families and to the improvement of public health, particularly during the childbearing and early childhood years. Megan earned a Bachelor of Arts degree from the University of Notre Dame and both a Master of Social Work and Master of Science in Public Health from The University of North Carolina at Chapel Hill.

Renée Boynton-Jarrett, a pediatrician and social epidemiologist, is an associate professor at Boston Medical Center and Boston University School of Medicine. She is the founding director of the Vital Village Networks. Vital Village uses a trauma-informed lens to improve community capacity to promote child wellbeing and advance equity through dedicated collaborative partnerships, research, data-sharing, and community leadership development in Boston and nationally through the NOW Forum and CRADLE Lab. Her scholarship has focused on early-life adversities as life course social determinants of health. She has a specific concentration on psychosocial stress and neuroendocrine and reproductive health outcomes, including obesity, puberty, and fertility. She is nationally recognized for work on the intersection of community violence, intimate partner violence, and child abuse and neglect and neighborhood characteristics that influence these patterns. She has received numerous awards for teaching, clinical care, and public health including the Massachusetts Public Health Association Paul Revere Award for outstanding impact on public health. She received her AB from Princeton University, her MD from Yale School of Medicine, and ScD in Social Epidemiology from Harvard School of Public Health, and completed residency in Pediatrics at Johns Hopkins Hospital.

Ana Cabello-De la Garza, MSW, MPH, is a senior program manager at UNC Health Sciences at MAHEC where she leads regional and statewide initiatives that equitably support communities to achieve their human right of optimal health throughout the life course. Her work revolves around inter-professional education, advocacy, research and policy. She is also the chair for the consumer work group of the National Preconception Health and Healthcare Initiative that focuses on sexual and reproductive health, health promotion, as well as disease prevention. Ana’s work is centered on health equity with a multi-dimensional lens that includes strategic planning, systems thinking, and collaborative research. Ana earned her masters of public health and social work at the University of North Carolina at Chapel Hill.

Chemyeeka Tumblin is an advocate, educator, and speaker. She received her Bachelor of Science in Biology with minors in Chemistry and Psychology from Georgia Southern University. She also holds a Master of Science in Public Health from Meharry Medical College and Masters in Marriage and Family Therapy from Trevecca Nazarene University. Chemyeeka has over 7 years experience in the field of behavioral health and is currently a Public Health Professional in the field of Maternal Child Health serving as a Project Coordinator with CityMatCH, a temp-licensed (post graduate under supervision) Marriage and Family Therapist in Nashville, Tennessee, as well as, a National Show Your Love ambassador, Postpartum Support International (PSI -TN) Tennessee Chapter Board Member, and a MaMa Glow Full Spectrum Doula trainee with Birth Manifesta.
The organizations that Chemyeeka are a part of are representation of her values, desires, and the communities in which she seeks to create change. In her personal life she is an advocate for Reproductive Justice and Mental Health, as well as, the Holistic Health Care needs of Black and Brown Communities. She enjoys speaking and educating on these topics, as well as serving as a resource to bring both awareness and access to her communities.

Eilish proudly represents Bronx, New York. She has always been known to be the more “radical” one in her family who, always sought fairness & justice. A deep thinker with a big heart Eilish strives to break the stereotypes associated with being a Black woman from the Bronx. Through her words and images, she hopes to inspire and encourage many women (and men) who look like her to explore different facets of this life and be more healthy. She has a Master’s of Public Health with a concentration in Sexual Reproductive Health and Maternal Child Health from the CUNY School of Public Health and has worked in Maternal Health for a decade. Currently, Eilish is pursuing her Master in Clinical Social Work at Hunter College Silberman School of Social Work. Her areas of interest include Preconception health especially for those who are over the age of 25 and mental health. Her loves include yoga, plants, the ocean, chocolate, belly dance & crafting.

Jussica C. Haynes, MPA, (she/her/hers), Jussica is an experienced health educator and is passionate about preconception health, interconception health, and sexuality education. She earned a Bachelor of Science in Public Health from East Carolina University and Master of Public Administration from North Carolina Central University. Jussica has taught comprehensive sexuality education at several middle and high schools in Chapel Hill-Carrboro, NC. She gained experience providing policy support for the statewide NC Early Childhood Action Plan at NC DHHS through research and data analysis. Jussica also has experience creating social media messages that promote well-being, positive parenting, breastfeeding, and self-sufficiency.
Currently, she is serving as the Perinatal & Lactation Education Coordinator for Improving Community Outcomes for Maternal and Child Health (ICO4MCH) at Mecklenburg County Public Health. She works collaboratively with community organizations in Charlotte, NC and Union County to promote the optimal health of people of childbearing age and to support normalizing breastfeeding in the community. Jussica aims to address barriers and intersectional inequalities faced by Black and Native communities to improve health outcomes.

Kennedy Bridges is a student at UNC-Chapel Hill pursuing a master’s degree in social work and public health. She is a trained full-spectrum doula and a reproductive justice advocate that supports birth, postpartum, lactation, pregnancy loss, abortion, and gender-affirming surgeries. Her extensive community work includes lactation support, violence prevention, harm reduction, peer education, and counseling. Currently, she works with the National Birth Equity Collaborative (NBEC) as a Birth Equity Program Associate on the Technical Assistance and Business Development team. She supports the project portfolio as a project manager and coordination of proposal development for new funding opportunities all in an effort to advance birth equity. Previously, Kennedy was a Business Development and Research analyst in the US Health Practice of Palladium International leading efforts to reduce maternal and infant health Inequities. She is a North Carolina native; a true Tar Heel who loves to cook, play videogames with her partner, and support growing families.

Sarah Verbiest, DrPH, MSW, MPH is the Director of the Jordan Institute for Families at the UNC School of Social Work and the Executive Director of the Center for Maternal and Infant Health at the School of Medicine.

Erin McClain, MPH, MA, is Assistant Director and Research Associate with the UNC Center for Maternal & Infant Health, where she brings over 15 years of experience facilitating and implementing perinatal systems change and quality improvement initiatives. She focuses broadly on the health of women of reproductive age, engaging in qualitative research with postpartum mothers and serving as a state coach for the HRSA-funded Preconception CoIIN and the MHLIC.

Katherine Bryant, MSPH, is a Research Associate and Project Manager for the UNC Center for Maternal and Infant Health and a Project Director in the UNC Jordan Institute for Families. Her portfolio includes serving as the project manager for a HRSA MCHB funded program – Improving Women’s Health: Preconception CoIIN.

Suzanne Woodward, BS, is the communications director at UNC Collaborative for Maternal and Infant Health. She specializes in health communications and digital media. She serves as the website/digital manager for numerous program and project websites, including ShowYourLoveToday.com, BeforeandBeyond.org and NewMomHealth.com.
Resources
Resources
 We recently launched a Future Forward in Preconception Health Webinar series. Live and pre-recorded sessions can be viewed here. Topics include sleep, fertility, cannabis, hypertension, diabetes, respectful care, and more.
We recently launched a Future Forward in Preconception Health Webinar series. Live and pre-recorded sessions can be viewed here. Topics include sleep, fertility, cannabis, hypertension, diabetes, respectful care, and more.
Click to register for the next event and watch our last webinar. Email Katherine_bryant@med.unc.edu for details.
 ShowYourLoveToday (SP) is an expert-written patient education resource on a variety of preconception health topics. This national resoruce is now available in Spanish. Click to view wellness resoruces topics, health insurance information, and newly updated COVID-19 guidance on getting pregnant. Patient education materials and tools are being developed and tested. More to come!
ShowYourLoveToday (SP) is an expert-written patient education resource on a variety of preconception health topics. This national resoruce is now available in Spanish. Click to view wellness resoruces topics, health insurance information, and newly updated COVID-19 guidance on getting pregnant. Patient education materials and tools are being developed and tested. More to come!
National Preconception Knowledge Survey – our team is surveying thousands of people across the nation to better understand preconception health knowledge, behaviors, and health care engagement. Email Katherine_Bryant@med.unc.edu for details. Results launched late-2021.
Updated Preconception Health Care CME Modules. We are in the process of updating all of our professional preconception health modules, with thanks to our partners for providing CME credit hours. New modules will launch fall 2021. Updated modules will be shared here.
Resources from various sessions –
Opportunity for Care:
- The Medicaid Coverage Gap and Maternal and Reproductive Health Equity
- The Commonwealth Fund interactive maps on state policies and maternal health
- Women’s Preventative Service Initiative (WPSI)
- Alliance for Innovation on Maternal Health (AIM) – AIM works through state and community-based teams to align national, state, and hospital level quality improvement efforts to improve overall maternal health outcomes.
- Office of Public Affairs Title X Family Planning Program
- The National Partnership for Women & Families and the National Birth Equity Collaborative are pleased to share the complete collection of bulletins from our series Saving the Lives of Moms and Babies: Addressing Racism and Socioeconomic Influencers of Health. We are also excited to announce the new social media toolkit, which includes shareable images for each of the series’ issue topics, sample tweets, Facebook and LinkedIn posts, and other resources for you to share and amplify this series.
Measuring & Indicators Session:
- Urban Institute – Do No Harm Guide
- Health Equity Style Guide, CDC reducing stigma
- Core State Preconception Health Indicators — Pregnancy Risk Assessment Monitoring System and Behavioral Risk Factor Surveillance System, 2009 CDC
- Racial Equity Data Roadmap, Mass.gov
- Health Care System Measures to Advance Preconception Wellness – Frayne et al
- Preconception Health Indicators for Public Health Surveillance – Robbins et al
- Making the Case: The Importance of Using 10 Key Preconception Indicators in Understanding the Health of Women of Reproductive Age – Kroelinger et al
- Disparities in Preconception Health Indicators — Behavioral Risk Factor Surveillance System, 2013–2015, and Pregnancy Risk Assessment Monitoring System, 2013–2014 – Robbins et al
- Core State Preconception Health Indicators — Pregnancy Risk Assessment Monitoring System and Behavioral Risk Factor Surveillance System, 2009 – CDC
- Surveillance Indicators for Women’s Preconception Care – Journal of Women’s HealthVol. 29, No. 7 Alys Adamski, Peter S. Bernstein, Sheree L. Boulet, Farah M. Chowdhury, Denise V. D’Angelo, Dean V. Coonrod, Daniel J. Frayne, Charlan Kroelinger, Isabel A. Morgan, Ekwutosi M. Okoroh, Christine K. Olson, Cheryl L. Robbins, Sarah Verbiest. Published Online:9 Jul 2020 https://doi.org/10.1089/jwh.2019.8146
- Callegari LS, Edmonds SW, Borrero S, Ryan GL, Cusack CM, Zephyrin LC. Preconception Care in the Veterans Health Administration. Semin Reprod Med. 2018 Nov;36(6):327-339. doi: 10.1055/s-0039-1678753. Epub 2019 Apr 19. PMID: 31003248.
Social Media & Inspiration Jamboard
Social Media & Inspiration Jamboard
Event Hashtag: #ShowYourLoveToday | Tag: @SYL_Today + @PCHHC on Twitter and @showyourlovetoday on Instagram + Facebook
Discussion/Inspiration Board: Add your ideas and thoughts to our event Jamboard. Click to add your note. 
Event Virtual Background: We welcome you to select one of our customized Zoom virtual backgrounds. Click here to download.
Drafted Messages:
Please join the Show Your Love Today Initiative for a national virtual summit, Future Forward: National Convening of Equity-Centered Women’s Wellness. Takes place on September 1st, 2nd and 15th from 12-4pm ET for each day. https://beforeandbeyond.org/futureforward/ #ShowYourLoveToday
What is next in ‘preconception health?’ Future Forward: National Convening of Equity-Centered Women’s Wellness is a free, virtual summit happening on September 1, 2, & 15 from 12-4pm ET each day. Registration & details: https://beforeandbeyond.org/futureforward/ #ShowYourLoveToday
Anyone interested in advancing women’s health and wellness is welcome to join the Future Forward: National Convening of Equity-Centered Women’s Wellness. This free, virtual event takes place on September 1st, 2nd and 15th from 12-4pm ET for each day. https://beforeandbeyond.org/futureforward/ #ShowYourLoveToday
ABOUT HRSA IM CoIIN PRECONCEPTION PROJECT: This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UF3MC31239-Providing Support For The Collaborative Improvement and Innovation Network (CoIIN) To Reduce Infant Mortality. The grant amount totals $1,494,993. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
 All women and men of reproductive age will achieve optimal health and wellness, fostering a healthy life course for them and any children they may have.
All women and men of reproductive age will achieve optimal health and wellness, fostering a healthy life course for them and any children they may have.